What We Treat
We Are Honored to Serve ALL Individuals With a Bleeding Disorder
Comprehensive Care for Bleeding Disorders
Hemophilia A
Hemophilia B
Carrier of Hemophilia
Von Willebrand's Disease
Platelet Deficiencies
Hereditary Hemorrhagic Telangiectasia
Glanzmann's Thrombasthenia
Other Rare Bleeding Disorders
Hemophilia A & B
What is Hemophilia?
TYPES
There are two main types of hemophilia: Hemophilia A is a deficiency of the clotting Factor 8 and Hemophilia B which is a deficiency in clotting Factor 9.
HOW COMMON
Hemophilia affects approximately 20,000 persons in the United States.
CAUSES
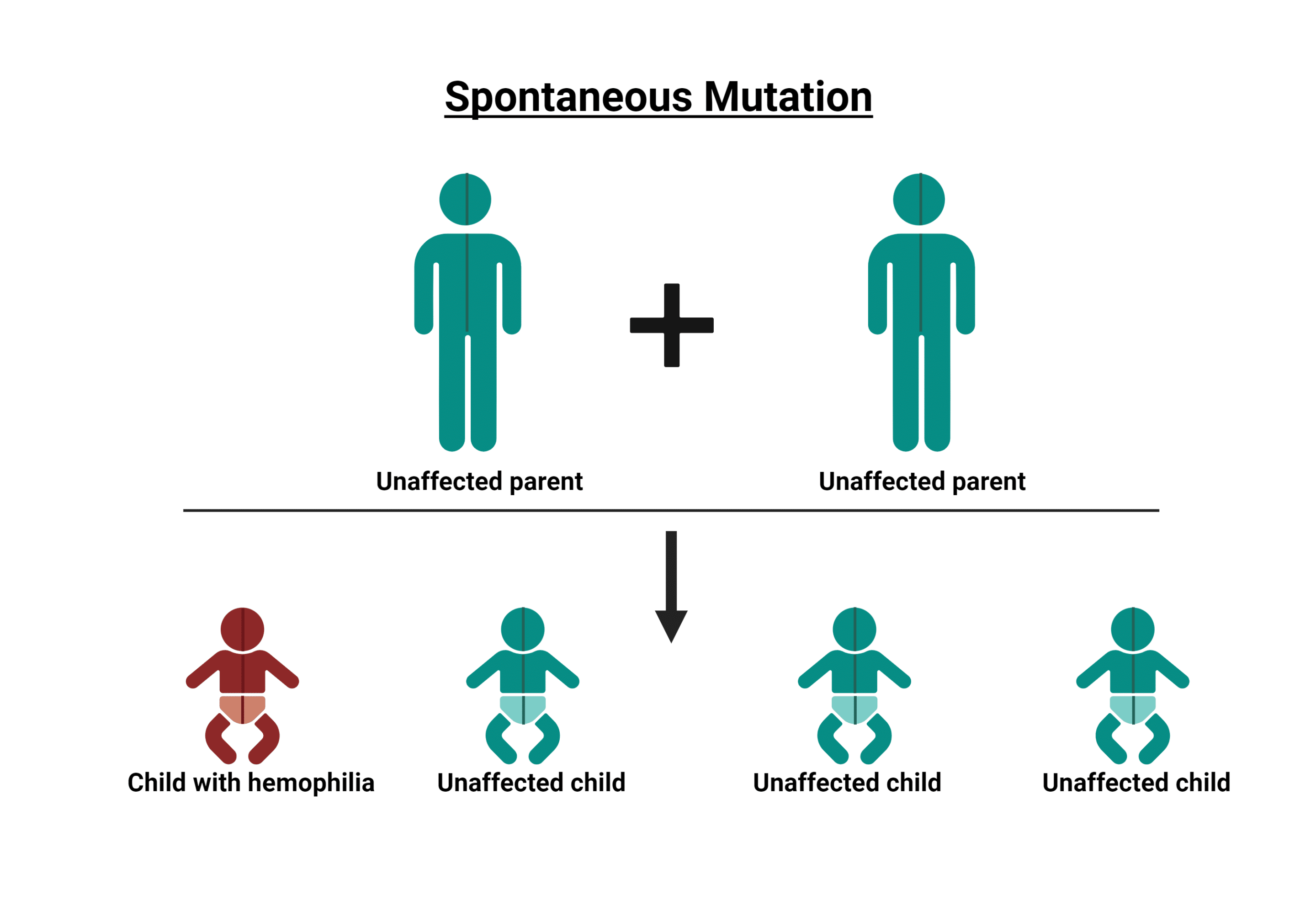
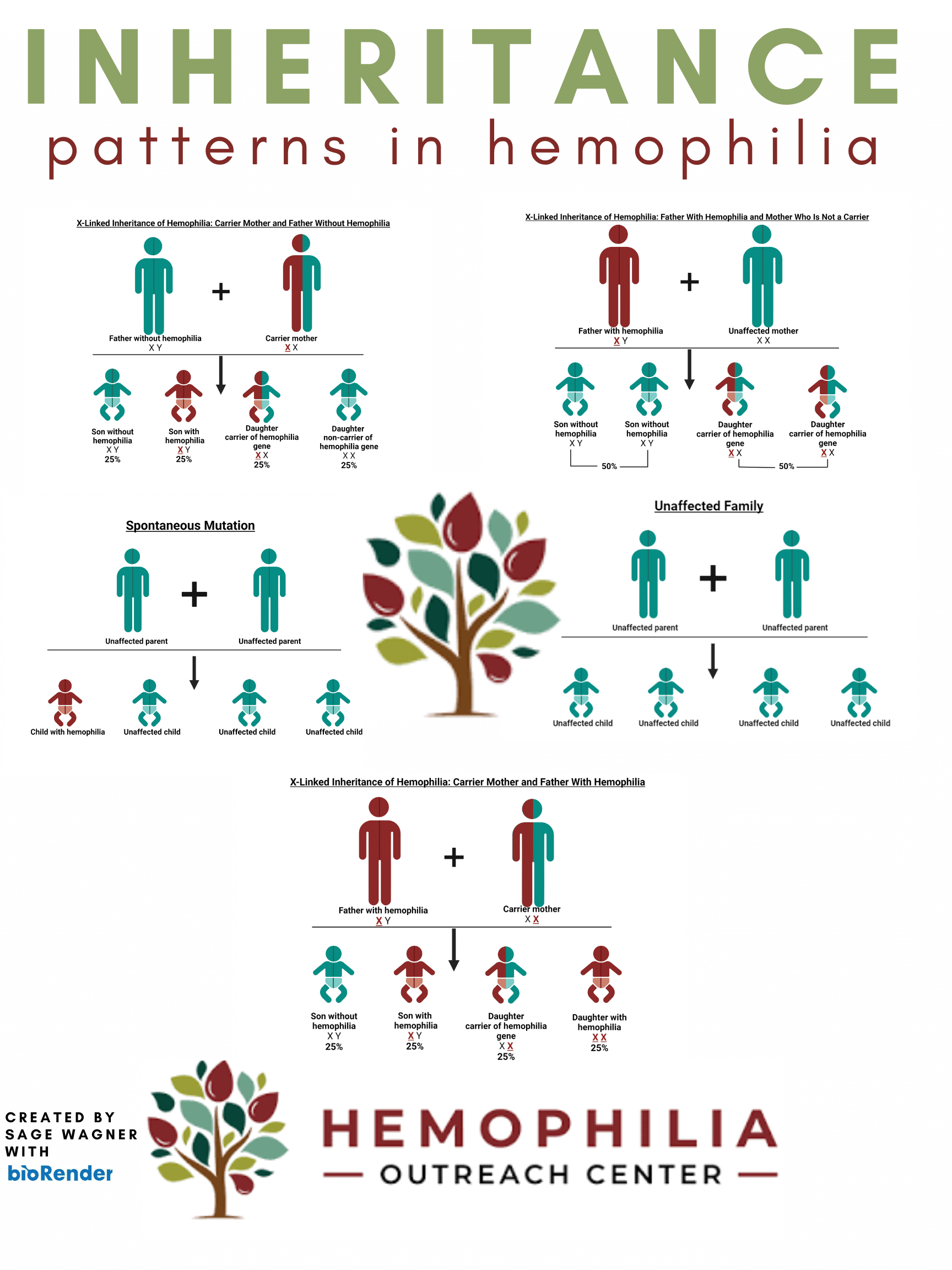
This genetic disorder is characterized by a missing or deficient clotting protein in the plasma, causing delayed clotting (prolonged bleeding). Hemophilia occurs almost exclusively in males. Men then pass the defective gene to their daughters who then become carriers of hemophilia. While there is an incidence of mutation, the genetic defect is carried on the X chromosome. As a result, women are carriers of hemophilia and can have the disorder and/or experience bleeding complications.
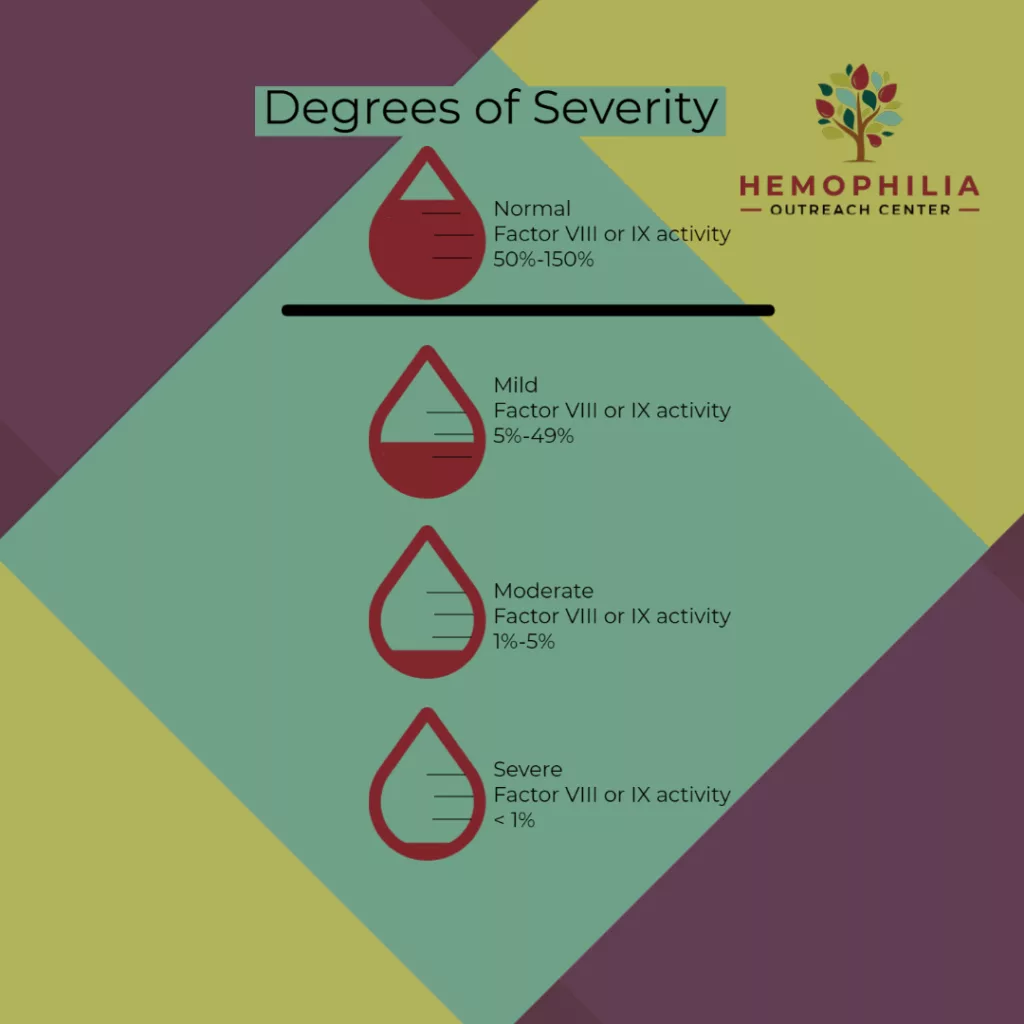
SEVERITY
Severity of Hemophilia A is determined by the percentage of Factor 9 found in the blood. Please note that hemophilia is very unique to each individual, and the bleeding may not relate to severity (A mild hemophiliac may have more bleeds than a severe)
- Mild – Between 5% and 40%
- Moderate – Between 1% and 5%
- Severe – <1%
SYMPTOMS
Individuals with hemophilia are at risk for bleeding after trauma, surgery, or dental work. They may also have internal or joint bleeding without an apparent cause. The more deficient you are of the clotting factor the more at risk you are for bleeding.
Carrier of Hemophilia
In about two-thirds of cases, there is a family history of hemophilia. Hemophilia doesn’t only affect those directly diagnosed with the condition; Carriers can experience symptoms and also can have levels that are considered as having hemophilia. At HOC, we provide valuable insights and support to carriers, helping you navigate the unique challenges and concerns that come with being a carrier of hemophilia. Our comprehensive care goes beyond traditional healthcare, ensuring that you receive the guidance and care you need to make informed decisions about you and your family’s health and well-being.
What is a Carrier of Hemophilia?
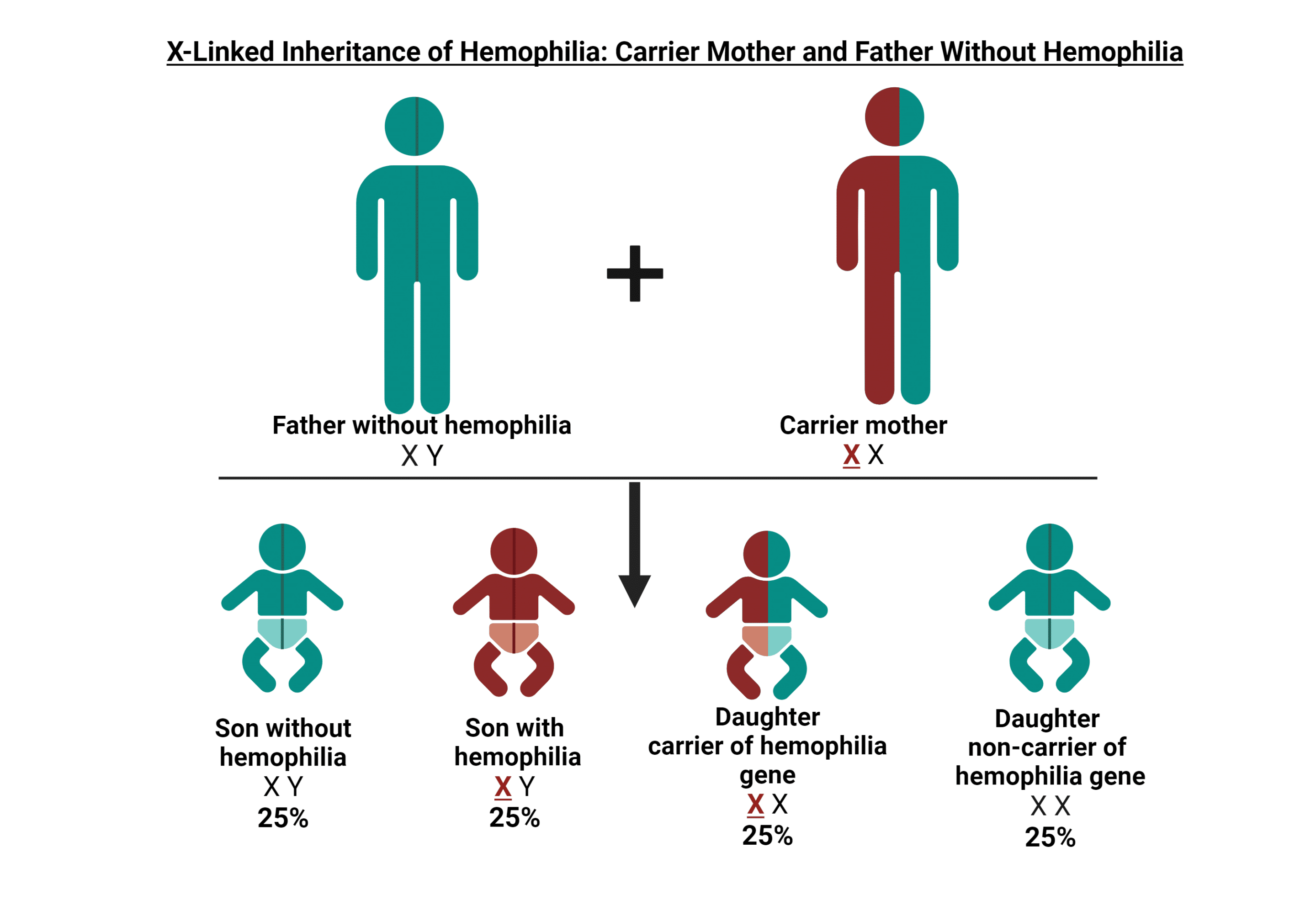
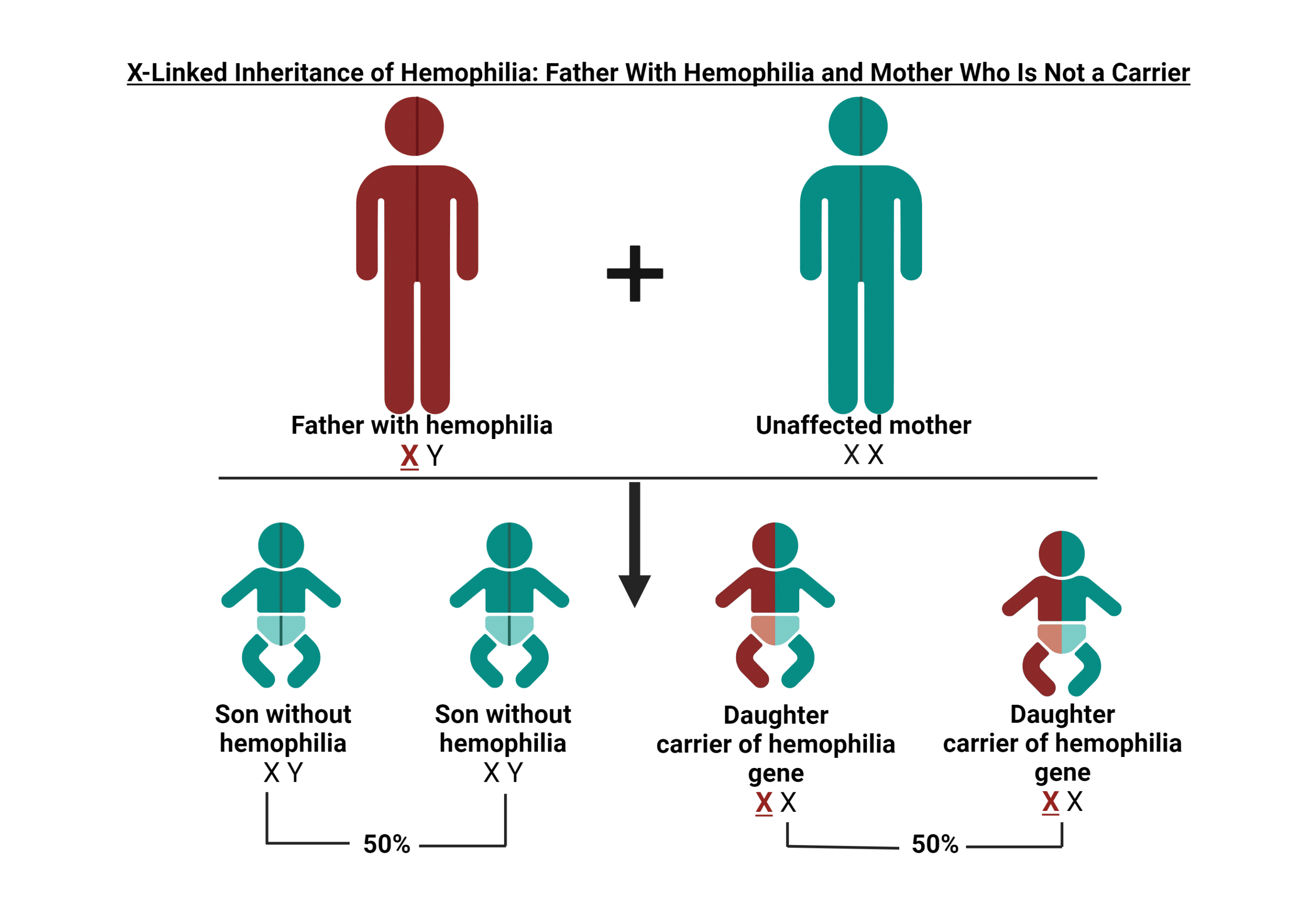
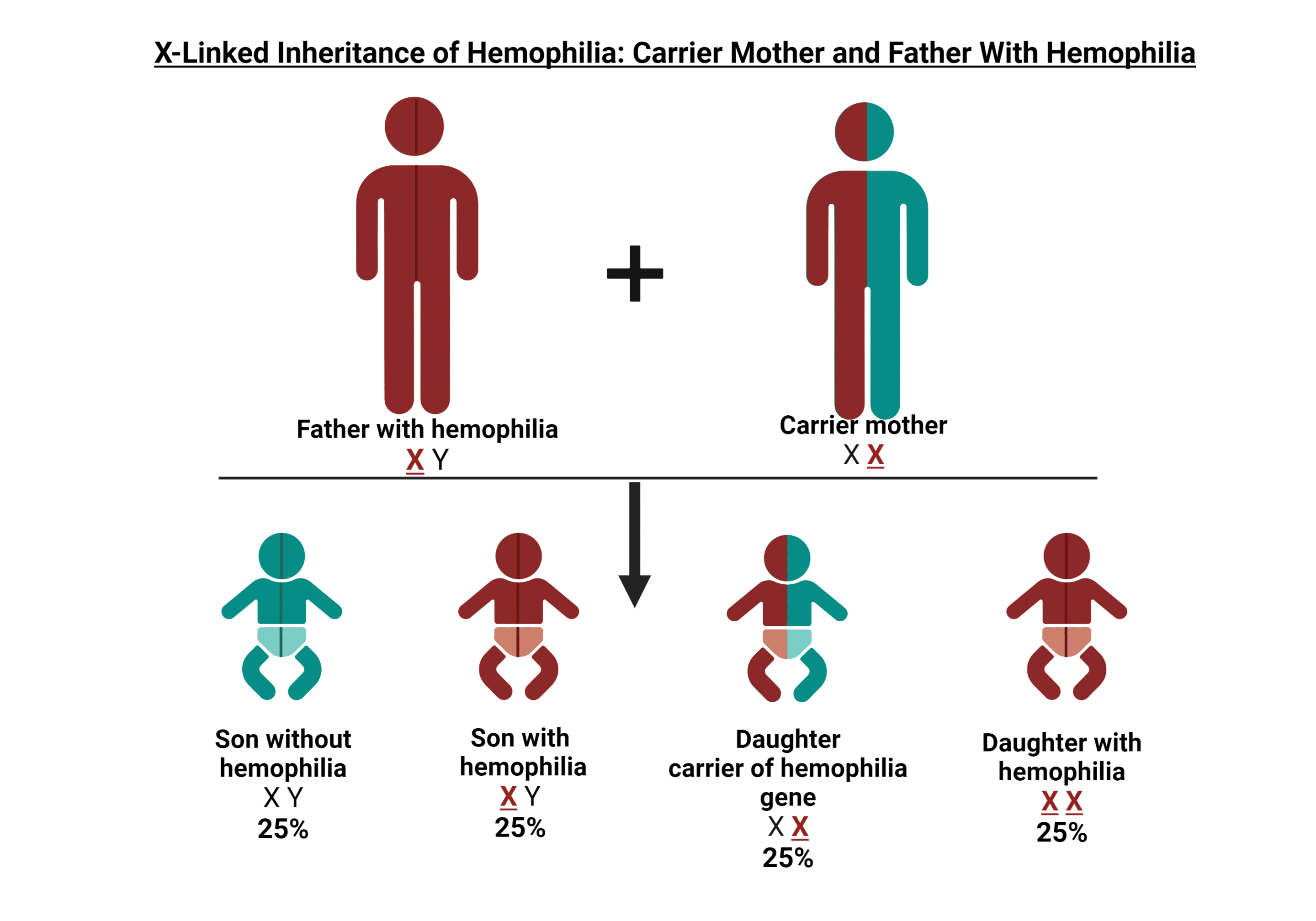
A hemophilia carrier is a female who has the gene that causes hemophilia A (Factor 8) or hemophilia B (Factor 9) deficiency. This genetic inheritance pattern helps us understand how hemophilia is passed down in families.
GENETIC INHERITANCE
The genes for hemophilia A & hemophilia B are carried on the X chromosome. Males have one X chromosome from their mother and one Y chromosome from their father (XY), while females inherit two X chromosomes, one from each parent (XX). Since the Y chromosome cannot help make Factor 8 or Factor 9 for normal blood clotting, if a boy inherits the X chromosome with the hemophilia gene from his mother, he will develop hemophilia.
Von Willebrand’s Disease
What is Von Willebrand's Disease?
The von Willebrand factor (VWF) is a protein in the blood that plays a crucial role in the blood clotting process. It serves as a bridge between platelets and the blood vessel walls, helping platelets adhere to the injured blood vessel and form clots to stop bleeding. VWF also carries and stabilizes a clotting factor called factor VIII, which is essential for blood clotting.
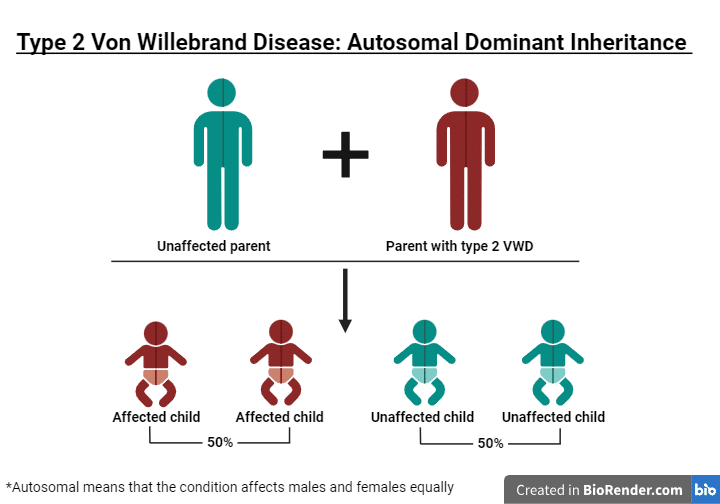
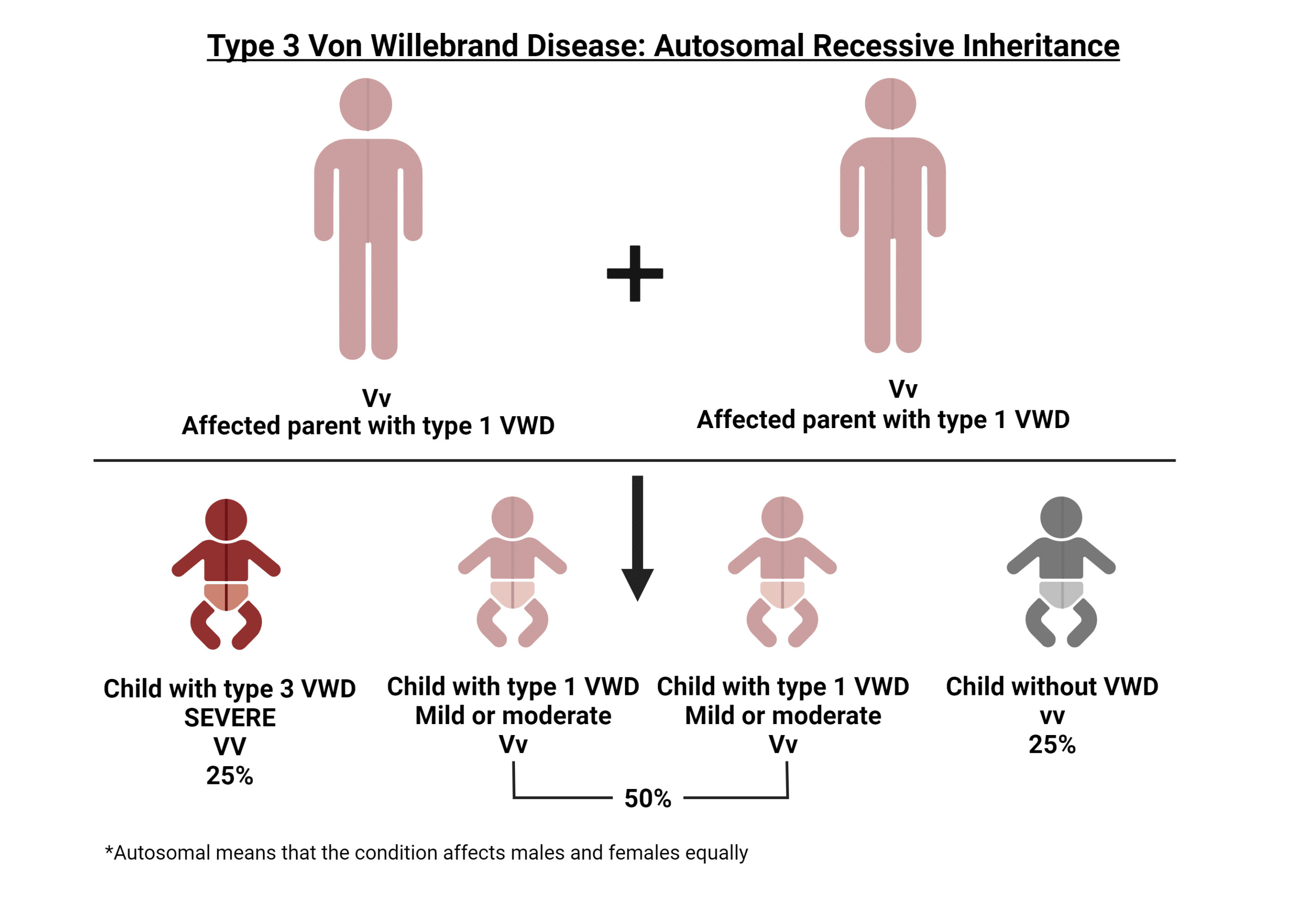
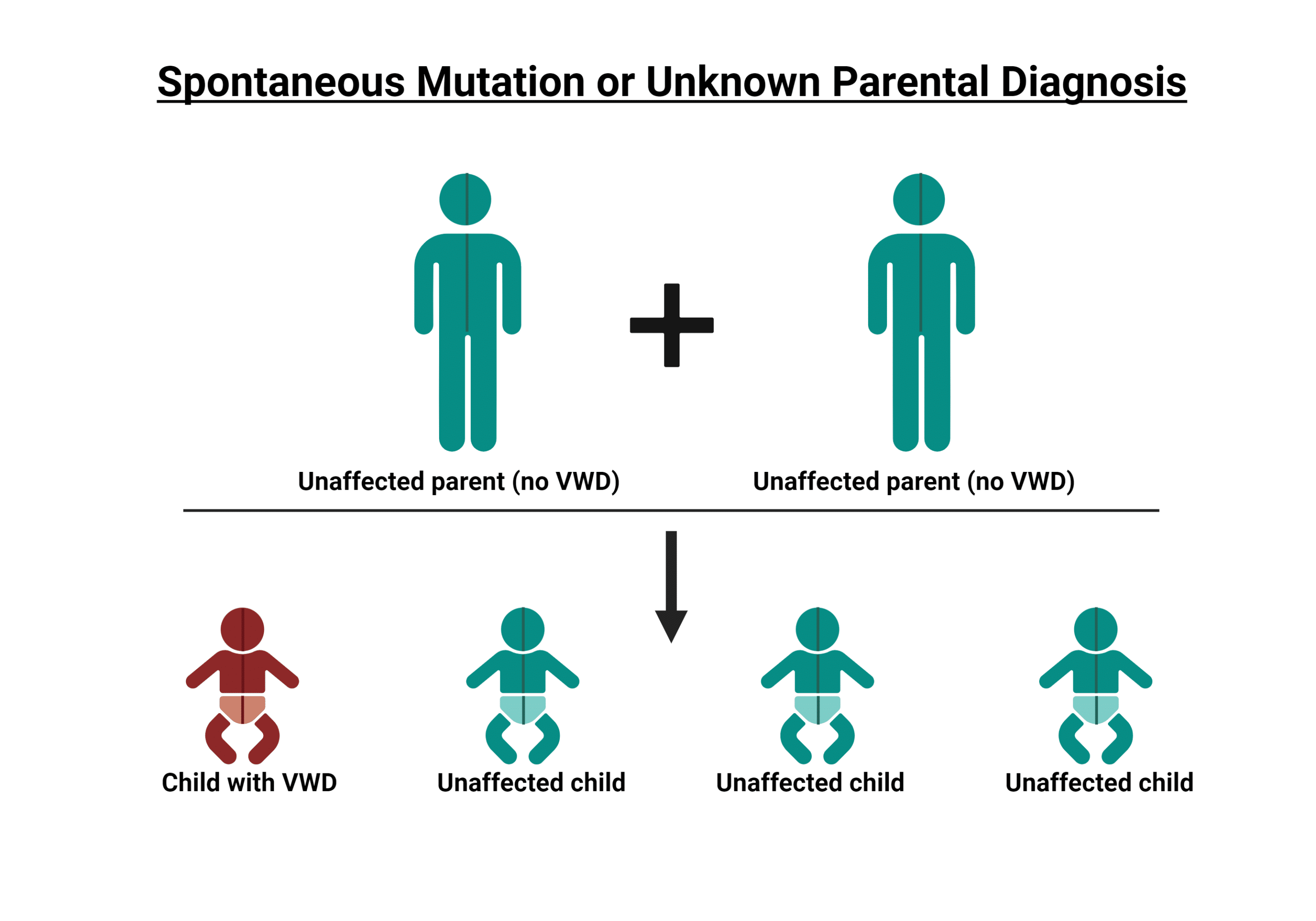
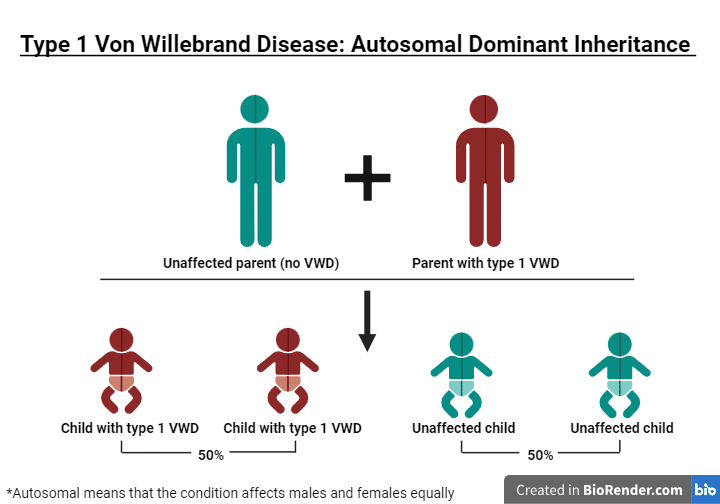
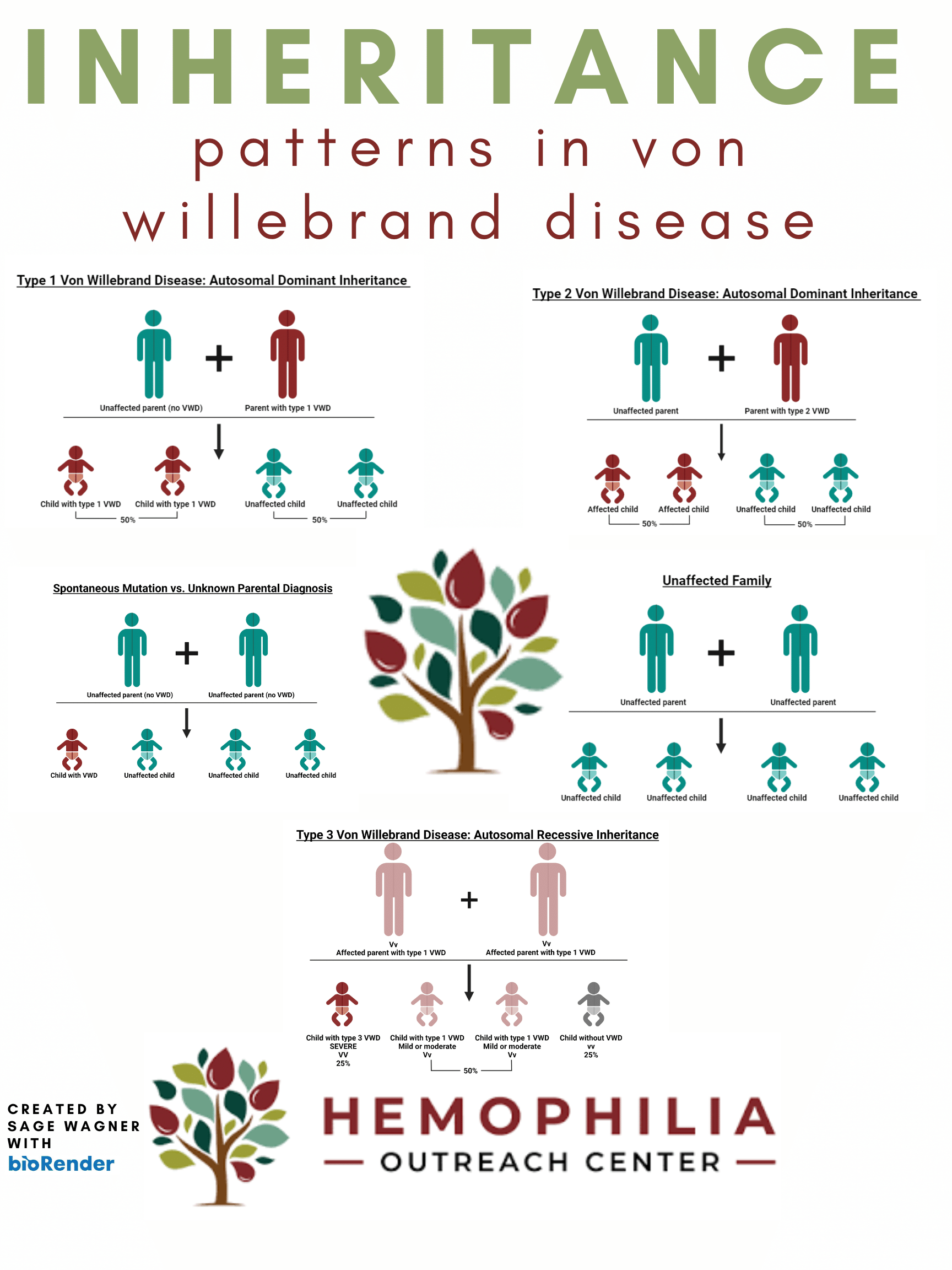
There are three main types of von Willebrand’s disease. Each type has at least one low lab result, but the types are differentiated by the multimers. Type 1 has normal multimers. Type 2 has abnormal multimers. Type 3 has an absence of multimers.
HOW COMMON
von Willebrand disease (vWD) is much more common, found in approximately 1-2% of the U.S. population. Like hemophilia, vWD is inherited from parent to child. The abnormal gene in von Willebrand’s disease is located on a chromosome called an autosome, which means that men and women can pass the defective gene to their children. Unlike hemophilia, vWD occurs equally in men and women.
SEVERITY
Individuals with von Willebands are at risk for prolonged nosebleeds, easy bruising, abnormal bleeding after surgery, dental work, or injuries. Women are more likely to experience symptoms of heavy or abnormal bleeding during their menstrual bleeding and after childbirth. Older patients are more susceptible to chronic gastrointestinal bleeding.
Platelet Deficiency
What is a Platelet Deficiency?
DEFINITION
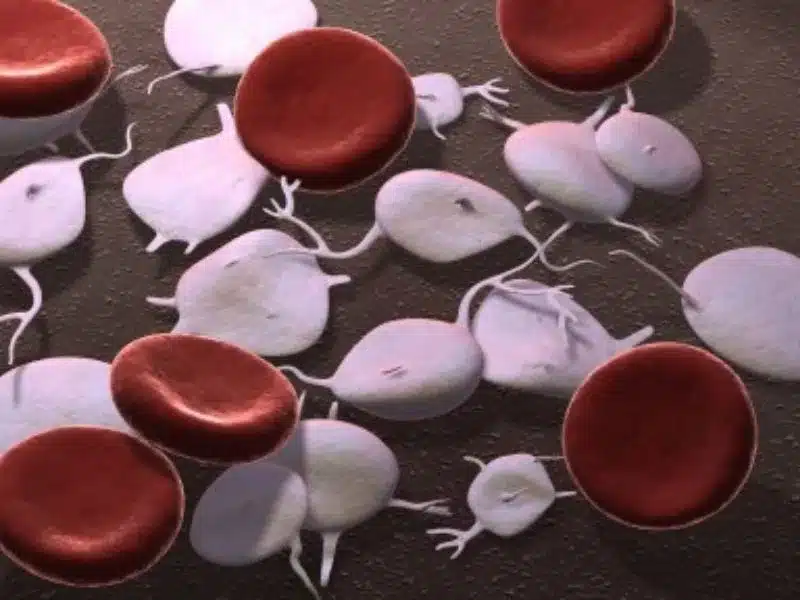
Platelets are a critical component of the blood clotting process. Platelets are small, disk shaped cells created in the bone marrow. Their primary role is to help the blood clot through adhesion aggregation activation and secretion. If there is a failure in any of the platelet functions there will be an increased tendency to bleed.
TYPES
Quantitative platelet disorder, which is the most commonly occurring type of platelet deficiency. There is a decrease in the number of platelets that function normally. Either the body doesn’t make enough OR the platelets get removed too quickly from the body.
Qualitative platelet disorder, this results from an abnormal structure or functioning of the platelet. The platelets are poor “quality”. Some potential causes include missing or abnormal proteins on the surface of the platelet membrane. Decinecry or defectiveness in the platelet granules or their contents (commonly referred to as storage pool disorder).
GENETIC INHERITANCE
Platelet deficiencies may or may not be genetically inherited, meaning you don’t need to have a family history to have a platelet disorder, but you could potentially pass the disorder onto your child.
Due to the complexity of platelet disorders, this is often difficult to diagnose.
SYMPTOMS
Individuals with a platelet disorder can experience easy bruising, nose bleeds, mouth or gum bleeds, heavy menstrual bleeding and after childbirth, and bleeding following dental work and surgery.

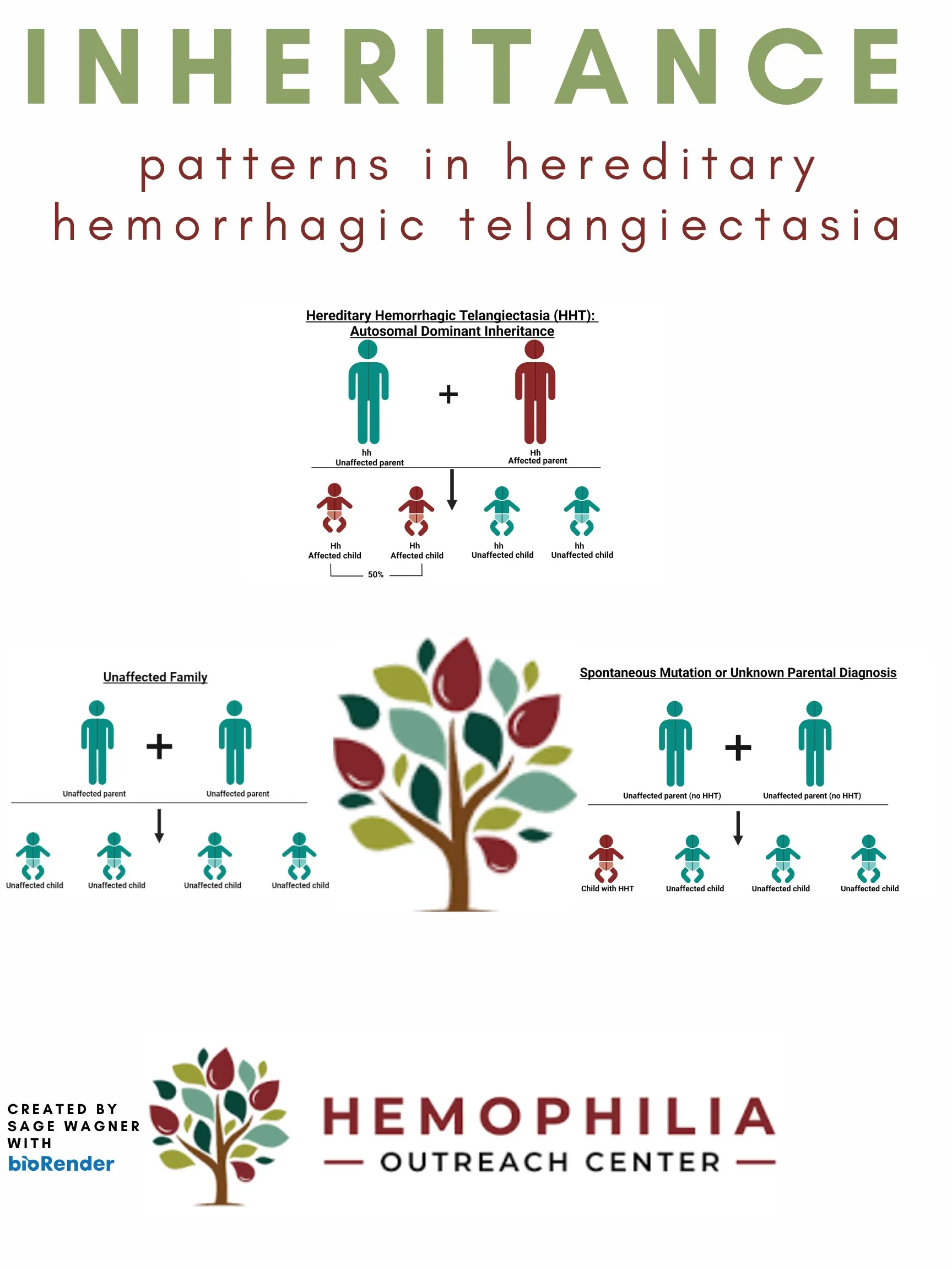
Hereditary Hemorrhagic Telangiectasia (HHT)
What is HHT?
DEFINITION
HHT is a disorder in which some blood vessels are not properly developed. A person with HHT can have malformed blood vessels, specifically blood vessels that lack capillaries. Capillaries are tiny blood vessels that connect arteries to veins.
SYMPTOMS
Without the capillaries – the tiny blood vessels that connect arteries to veins – the arteries attach directly to the veins resulting in increased pressure. This increased pressure can result in bleeding at these sites. HHT is commonly referred to as Osler-Weber-Rendu (OWR),the names of several doctors who studied HHT in the 1800’s.
The most common symptom in patients with HHT is nosebleeds that may or may not persist throughout the person’s life. These nosebleeds occur in about 90% of patients at some point in their life. Nosebleeds may be very infrequent and can be easily stopped or occur multiple times daily.
HOW COMMON
HHT affects approximately 1 in 5000 people.
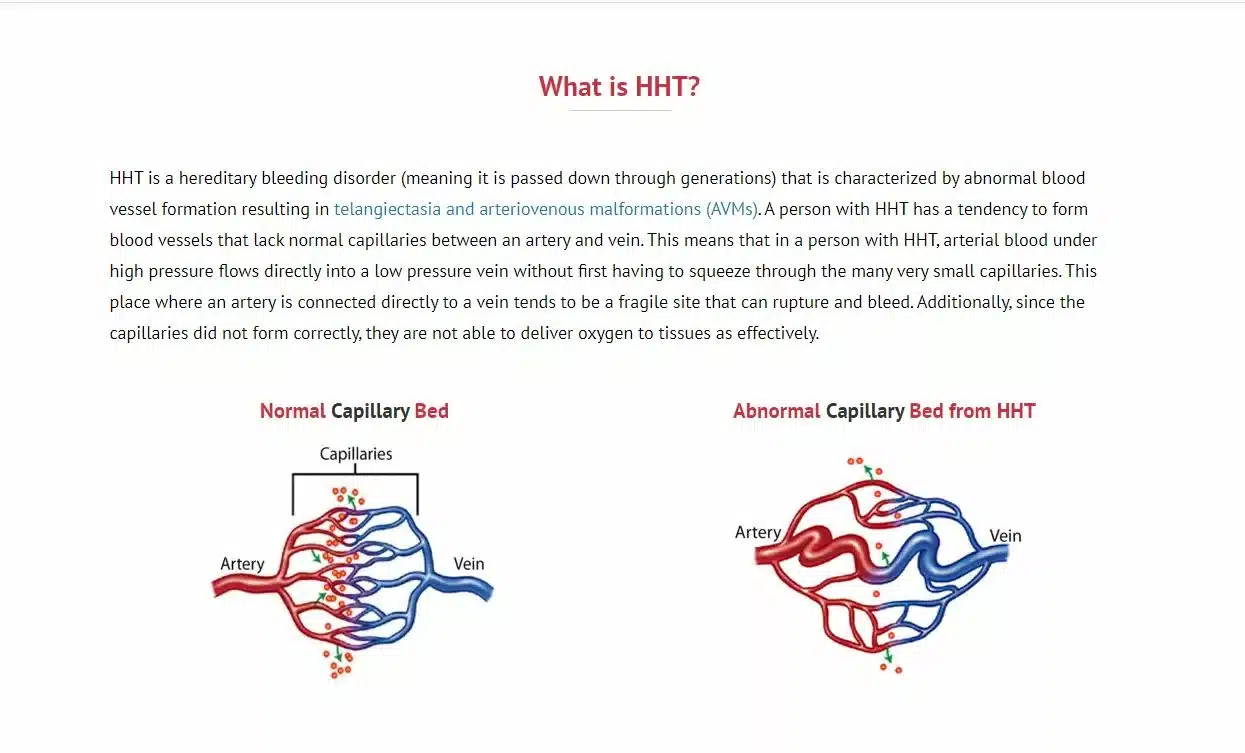
Image Credit: CureHHT
Glanzmann’s Thrombasthenia
Glanzmann's Thrombasthenia
Other Rare Bleeding Disorders
Hemophilia Outreach Center is your dedicated ally in diagnosing and managing rare bleeding disorders, including Factor 7 deficiency, Acquired Hemophilia, Acquired von Willebrand’s disease and other rare disorders. Our focus is on positive patient outcomes and improving your quality of life. Whether you need clinical treatment, support for reducing bleeding risks, genetic counseling, or a connection with a supportive community, HOC is here to empower you to thrive.
What other bleeding disorders do we treat?
FACTOR 7 DEFICIENCY
Factor 7 deficiency is a rare genetic disorder caused by a deficiency or reduced activity of clotting factor 7. This is considered to be the most common of the rare bleeding disorders. It is estimated to occur in every 1 of 300,000-500,000. It is inherited in an autosomal excessive fashion meaning both parents must carry the gene to pass it on to their child. This affects men and women equally. (citation)
Individuals with factor 7 deficiency are at risk for bleeding after trauma, surgery, or dental work. They may also have internal or joint bleeding without an apparent cause. The more deficient a person is in the clotting factor the more at risk they are for bleeding.
Women are more likely to experience symptoms of heavy or abnormal bleeding during their menstrual bleeding and after childbirth.
ACQUIRED HEMOPHILIA
Acquired Hemophilia is an autoimmune disease. The antibodies from the immune system attack and destroy one of the body’s clotting factors (most often clotting factor 8). This can lead to excessive bleeding and can affect males and females equally.
Acquired hemophilia can be caused by other autoimmune diseases, cancer, pregnancy, or certain drugs but other times there is no known cause. Acquired hemophilia is extremely rare only affecting approximately 1 of 1,000,000 people.
ACQUIRED VON WILLEBRAND’S DISEASE
The immune system can also attack von Willebrand factor, resulting in acquired von Willebrand’s disease.
UNSPECIFIED BLEEDING DISORDER
Individuals with Unspecified bleeding disorders can experience prolonged or excessive bleeding. This may occur spontaneously, after an injury, or during/following a surgical procedure.
In these situations, although testing is done for all bleeding disorders, there are no abnormal lab results that lead to a specific bleeding disorder diagnosis.
Patients typically present with post surgical/dental bleeding, bruising from minor trauma, nose bleeds, and/or heavy menstrual cycles.
Inheritance for unspecified bleeding disorders is unknown.
Treatment for bleeding prior to procedures may be required even without a formal diagnosis. It is very important that you discuss your abnormal bleeding history with all care providers and make sure HOC is involved in your care.

How We Can Assist You in Your Bleeding Disorder Journey
Through our comprehensive care and a wide range of health services for bleeding disorders, we empower our patients to live full and meaningful lives. Learn more about our services and how we can assist you in your hemophilia journey.